Oral Surgery Information
Oral surgery is a specialized area of dentistry that involves surgical procedures related to the mouth, jaw, and face. Common oral surgeries include tooth extractions, wisdom teeth removal, dental implants, corrective jaw surgery, and treatment of oral diseases and injuries. Before undergoing any oral surgery, it's important to have a thorough consultation with a qualified oral surgeon to discuss the risks, benefits, and expected outcomes of the procedure. Depending on the type of surgery, patients may require local anesthesia, sedation, or general anesthesia to ensure their comfort during the procedure. After surgery, patients will receive detailed instructions on how to care for the surgical site and manage any discomfort or swelling. With proper care and attention, most oral surgeries have a high success rate and can help patients achieve better oral health and function.
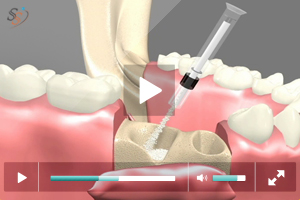
Bone Grafting
Extraction of a tooth causes resorption of the supporting bone. Bone resorption causes a 40-60% decrease in its width during the first three years following extraction. Bone resorption occurs at the expense of the outer plate of bone reducing the width of bone. Then overtime the height of bone is reduced. This becomes critical for anterior implants where ideal aesthetics, phonetics and function is desired. In the upper jaw following extraction the sinus floor begins to expand further decreasing the available bone to place implants in the posterior maxilla. In the lower jaw the mandibular nerve runs in the bone limiting the length of the implant placed.
Bone Grafting can be used as a socket preservation procedure when it is placed following extraction of a tooth or to augment an atrophied or reabsorbed site.
Bone Grafting Procedures
Ridge-augmentation
In severe cases of ridge resorption bone graft is placed to increase the ridge height and or width.
Sinus Lift and Graft Procedure
This procedure involves elevating the sinus membrane and placing the bone graft onto the sinus floor, allowing implants to be placed in the back part of the upper jaw.
Nerve - repositioning
The mandibular nerve may need to be moved in order to make room for placement of dental implants in the lower jaw.
These procedures may be performed separately or together, depending upon the individual's condition. There are several areas of the body which are suitable for attaining bone grafts. In the maxillofacial region, bone grafts can be taken from inside the mouth, in the area of the chin or third molar region or in the upper jaw behind the last tooth. In more extensive situations, a greater quantity of bone can be attained from the hip or the outer aspect of the tibia at the knee.
Several bone augmentation materials are available to stimulate and encourage bone growth in areas where it is lost as a result of pathological or physiological processes.
Bone grafting materials can be derived from various sources
- Allograft materials derived from cadaver bone of the same species
- Autogeneous material derived from the recipient's intra-oral or extra-oral site
- Alloplastic materials are exclusively derived from synthetic sources
- Xenografts derived from the inorganic portion of animal bone
Bone Grafting will help to place larger diameter implants in ideal locations that are stable and serviceable for a long time. It also helps to establish normal volume and dimensions of bone for ideal aesthetics, lip support and phonetics.
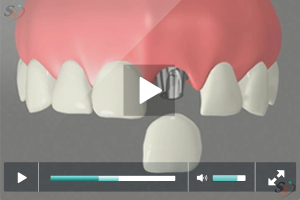
Dental Implants
When a tooth is lost the specialized bony process that houses the tooth begins to reabsorb due to lack of stimulation. This causes a decrease in width and height of the bone in the area the tooth is lost. Neighbouring teeth and opposing teeth begin to move into the space. This causes food lodgement, subsequent decay, gum disease and abnormal forces being transmitted to teeth leading to fracture of cusps which may necessitate root canal treatment or extraction. Loss of teeth can also cause the cheek and lips to collapse giving an aged look.
The consequences of tooth loss can be prevented by replacing the lost tooth in a timely manner. Although there are several options to replace a missing tooth the number one choice for replacing lost teeth are dental implants. Implants are tiny titanium screws or posts that are surgically placed in the bone. Once integrated into bone they act like roots onto which small posts are attached which protrude through the gums. These posts provide stable anchors to the replacement teeth. Implants maintain the bone height by stimulation and prevents unnecessary trimming of adjoining teeth for bridge placement. Since implants are titanium posts there is no chance for decay on implants. Implants can service you for several years with regular professional cleaning and proper home care.
Many people who are missing a single tooth opt for a fixed bridge; but a bridge may require the cutting down of healthy, adjacent teeth that may or may not need to be restored in the future. Then there is the additional cost of possibly having to replace the bridge once, twice or more over the course of a lifetime due to decay or gum problems affecting the anchor teeth.
Another option to replace missing teeth is a removable partial denture or complete denture depending on the number of teeth missing. The chewing efficiency with a denture is reduced to more than half of that of natural teeth. The teeth that support the partial denture are weakened due to the excessive loads acting on them and eventually are lost. The denture rests on the gum causing tissue abrasion and bone loss. Removable dentures may slip or cause embarrassing clicking sounds while eating or speaking.
Studies show that within five to seven years there is a failure rate of up to 30% in teeth located next to a fixed bridge or removable partial denture.
Who is a candidate for Implants?
Anyone who is missing one or several teeth is a candidate for implants. With the exception of growing children, dental implants are the solution of choice for people of all ages, even those with the following health concerns:
Existing Medical Conditions: If you can have routine dental treatment, you can generally have an implant placed. While precautions are advisable for certain conditions, patients with such chronic diseases as high blood pressure and diabetes are usually successful candidates for dental implant treatment.
Gum Disease or Problem Teeth: Almost all implants placed in patients who have lost their teeth to periodontal disease or decay has been successful.
Currently Wearing Partials or Dentures: Implants can replace removable bridges or dentures, or they can be used to stabilize and secure the denture, making it much more comfortable.
Smokers: Although smoking lowers the success rate of implants, it doesn't eliminate the possibility of getting them.
Bone Loss: Bone loss is not uncommon for people who have lost teeth or had periodontal disease. Oral and maxillofacial surgeons are trained and experienced in grafting bone to safely and permanently secure the implant.
Implant tooth replacement in children is usually deferred until their jaw growth is complete. There are, however, some instances when a dental implant may be appropriate, such as when it is part of the child's orthodontic treatment plan. Your family dentist or orthodontist can guide you in this instance.
Procedure
Dental Implant placement usually takes two surgical appointments:
- During the first surgical appointment the implant site is prepared to receive the implant following strict aseptic procedures. The selected size of the implant is placed in the prepared site. The gum tissue is sutured over the implant. The implant takes 4- 6 months to fuse with the bone.
- During the second surgical appointment the implant is uncovered and the appropriate post is attached to which the replacement tooth is anchored. An impression of the post is taken and sent to the lab for the fabrication of the implant crown. During this time a temporary crown is placed. Once the final crown is back it is cemented with permanent cement.
Wisdom Teeth
Wisdom teeth also referred to as third molars usually erupt between 17-25 years of age. Anthropological studies show that wisdom teeth erupt in order to compensate for the excessive wear and forward drifting of teeth due to the rough diet of early humans. Modern diet is soft and refined and excessive wear of teeth is not observed. As a result there is no room for wisdom teeth to erupt. This causes the wisdom teeth to get impacted.
What is an impacted tooth?
A tooth becomes impacted when there is a lack of space in the dental arch and its growth and eruption are prevented by overlying gum, bone or another tooth. A tooth may be partially impacted, which means a portion of it has broken through the gum, or totally impacted when it is unable to break through the gum at all.
What are the problems associated with impacted wisdom teeth?
There are numerous problems depending on the type of impaction. Partially impacted wisdom teeth cause the overlying gum tissue to become inflamed and irritated. There will be food lodgment in the area which will eventually lead to decay on both the wisdom tooth and the tooth next to it .Failure to remove the wisdom tooth in a timely manner will necessitate root canal treatment on the tooth adjacent to it. Also the area can get infected and the infection can spread to the muscles that help to open and close the mouth leading to restricted opening of the mouth, stiffness and illness. The pressure from the erupting wisdom tooth may move other teeth and disrupt the alignment of teeth.
When the wisdom tooth is totally impacted the developmental sac that surrounds the tooth becomes filled with fluid and enlarges to form a cyst. As the cyst grows it may hollow out the jaw and permanently damage adjacent teeth, the surrounding bone and nerves. Rarely, if a cyst is not treated, a tumor may develop from its walls and a more serious surgical procedure may be required to remove it. Sometimes the wisdom teeth make their way through the gum tissue but due to lack of space may erupt more buccally (towards your cheek) or ligually (towards your tongue). This causes cheek biting, food lodgment, subsequent decay and infection.
Early removal is recommended to avoid such problems and to decrease the surgical risks involved with the procedure.
How early should wisdom teeth be removed?
Wisdom teeth are easier to remove when the patient is younger, since their roots are not completely formed, the surrounding bone is softer, and there is less chance of damaging nearby nerves or other structures. Removal of wisdom teeth at a later age becomes more complicated as the roots have fully developed (may involve the nerve), and the jawbone is denser. Also early removal will ensure optimal and less complicated healing. For some patients the wisdom teeth may erupt normally and will be properly aligned in the arch. In such instances the wisdom teeth can be retained with proper home care.
Procedure for removal of wisdom teeth
Most wisdom tooth extractions are performed in the oral and maxillofacial surgery office under local anesthesia, intravenous sedation or general anesthesia. Your oral and maxillofacial surgeon will discuss the anesthetic option that is right for you.
The extent of the procedure depends on the tooth position, degree of impaction and root development. Once adequate anesthesia is achieved an incision is made in your gums adjacent to the probable location of the wisdom tooth to be removed. The gum tissue overlying the impacted tooth is reflected. Removal of some bone around the tooth may be necessary to free the tooth and aid in a non-traumatic extraction. Resorbable sutures may be placed.







.jpg)
.jpg)
